
New York: Pearson/Longman.The Subjective, Objective, Assessment and Plan (SOAP) note is an acronym representing a widely used method of documentation for healthcare providers. Journal of Counseling & Development, 80, 286-292. Learning to write case notes using the SOAP format. Min, mod, max- minimum, moderate, maximumĬameron, Susan & turtle-song, imani.
I.e.- id est, use when giving alternative explanation or wording
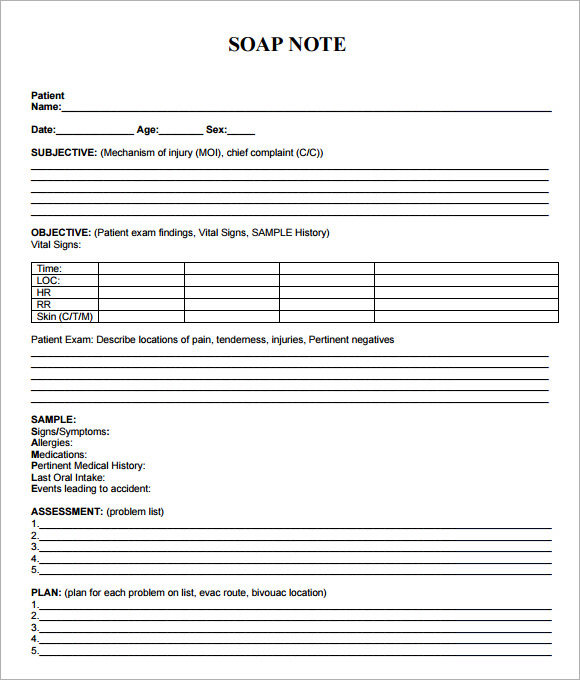
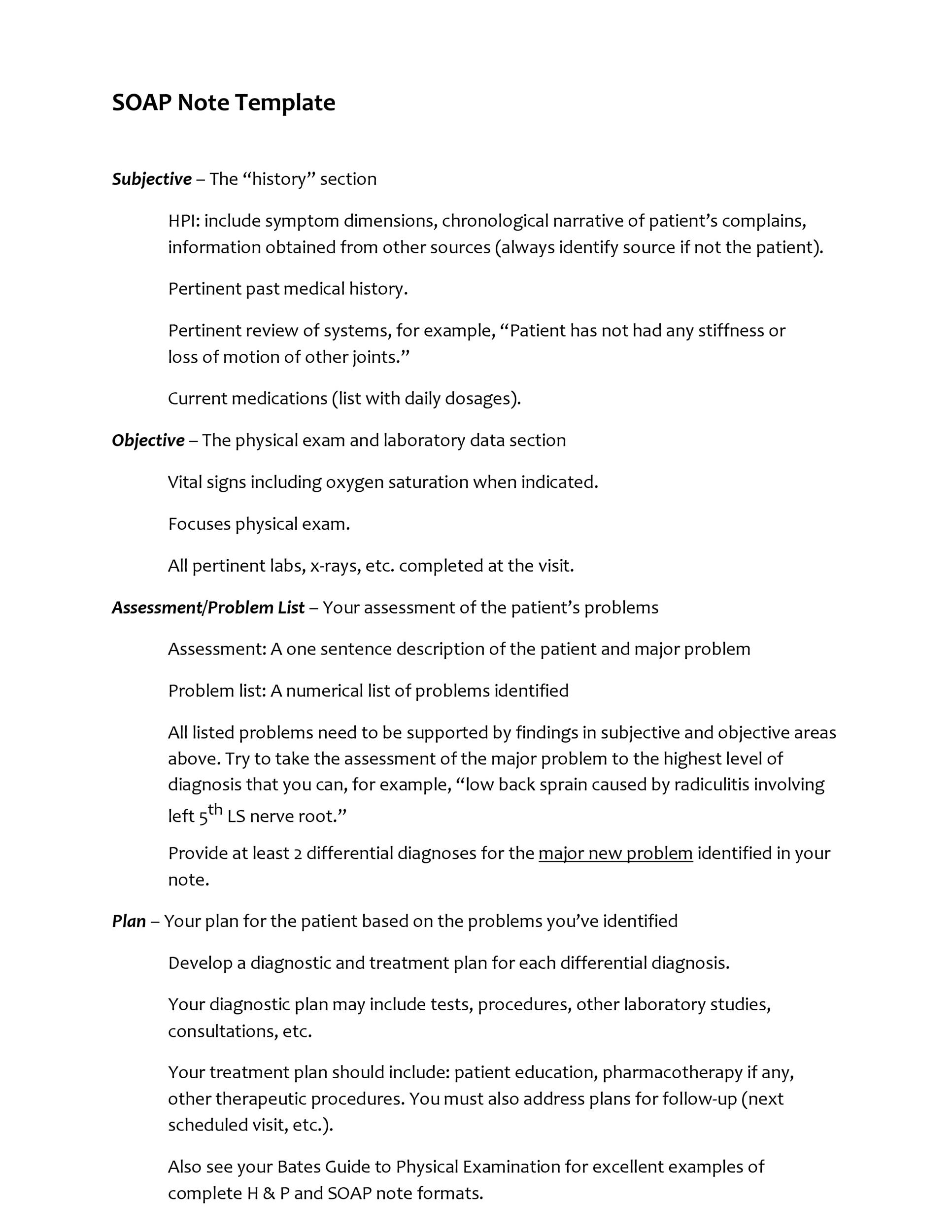
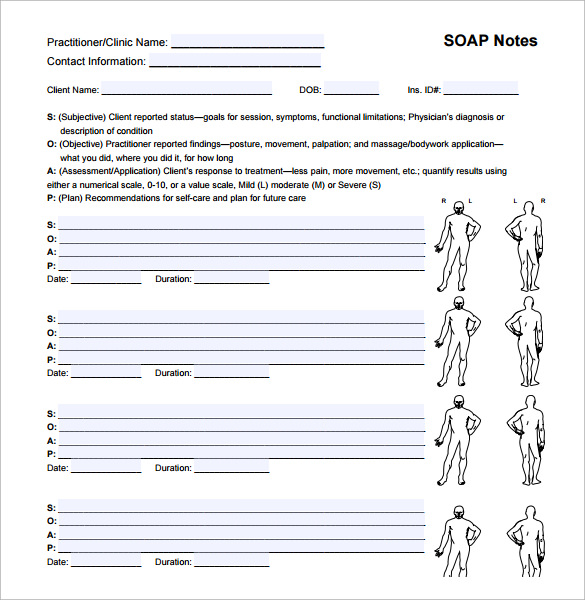
Some commonly used abbreviations for SOAP notes are:Į.g.- exempli gratia, use when giving an example In some settings, especially those that use electronic healthcare records, the writer will be constrained to a predetermined number of characters that can be entered. It is perfectly acceptable and often encouraged in many settings to use abbreviations when writing SOAP notes. To save both the writer and reader time, avoid overly wordy phrasing and unnecessary detail. Conversely, also keep in mind that efficiency and time management are important in the healthcare professions. As mentioned above, different fields and even different clinics will have varied preferences and practices for writing these clinical documents.ĭespite this variation, it is important to keep in mind that a SOAP note should be sufficiently detailed so that an outside healthcare provider with no previous interaction with the patient/client can obtain all the necessary information from the session or incident documented to appropriately provide care for the patient/client. Rather, they showcase differences in approaches for SOAP note styles. These examples are not the only two ways to write a SOAP note. Next session, introduce use of “time-outs.” S. Refer to Men’s Alternatives to Violence Group. Clinical impressions: rule out Intermittent Explosive Disorder given bouts of uncontrolled rage with non-specific emotional trigger. ( A) Physical Abuse of Adult and Child(ren). Toward the end of the session stood up, with clenched fists and jaw, angrily stated that counseling is “same old B.S.!” Rushed out of office. ( O) Generally agitated throughout the session. Personal history: childhood physical and mental abuse resulting in foster care placement, ages 11-18. Recent history: States he met and verbally fought with his wife yesterday regarding the privileges of oldest child. Insists the use of violence has been needed to “straighten out” family members. ( S) Reports counseling is not helping him get his family back. The second is an example from a mental health counseling setting. The first come from within a hospital context. Note the difference in style and format in the following two examples.
#Soap notes full#
SOAP notes can be written in full sentence paragraph form or as an organized list of sentences fragments.
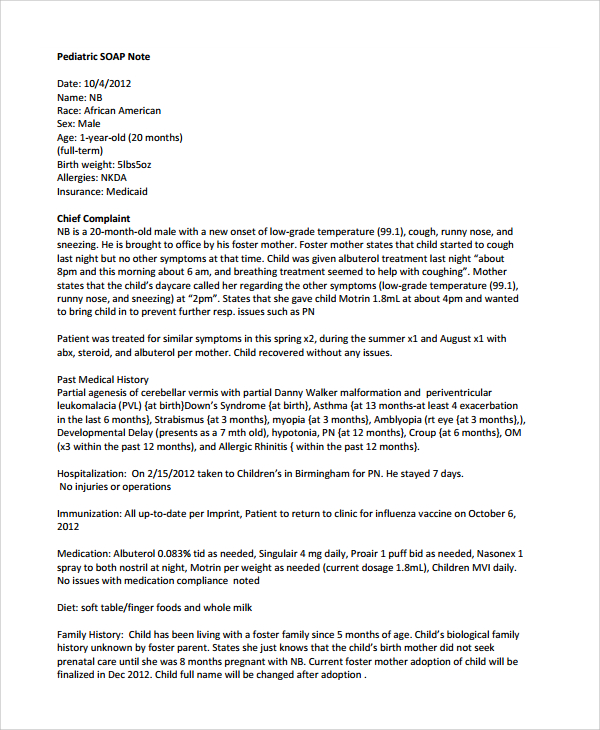
The length and style of a SOAP note will vary depending on one’s field, individual workplace, and job requirements. How long is a SOAP note and how do I style one? A good SOAP note should result in improved quality of patient care by helping healthcare professionals better document and therefore recall and apply details about a specific case. The audience of SOAP notes generally consists of other healthcare providers both within the writer’s own field as well in related fields but can also include readers such as those associated with insurance companies and litigation. A SOAP note should convey information from a session that the writer feels is relevant for other healthcare professionals to provide appropriate treatment. However, all SOAP notes should include Subjective, Objective, Assessment, and Plan sections, hence the acronym SOAP. Because SOAP notes are employed by a broad range of fields with different patient/client care objectives, their ideal format can differ substantially between fields, workplaces, and even within departments. What is a SOAP note?Ī SOAP note is a form of written documentation many healthcare professions use to record a patient or client interaction. The resource discusses the audience and purpose of SOAP notes, suggested content for each section, and examples of appropriate and inappropriate language. This resource provides information on SOAP Notes, which are a clinical documentation format used in a range of healthcare fields. Writing Letters of Recommendation for Students.


 0 kommentar(er)
0 kommentar(er)
